When experiencing menstrual changes – from PMS to menopause – women are often confused about the differences between natural, synthetic and bioidentical hormones. With more than 48 million women going through The Change at the same time, it’s important for them to understand their choices and whether or not they need Hormone Replacement Therapy (HRT).
When experiencing menstrual changes – from PMS to menopause – women are often confused about the differences between natural, synthetic and bioidentical hormones. With more than 48 million women going through The Change at the same time, it’s important for them to understand their choices and whether or not they need Hormone Replacement Therapy (HRT).Natural Hormones come from a plant, mineral, or animal source. They are not easily, if ever, converted to an identical match to those found in the female body. Products in this category include prescription HRT formulas and over-the-counter soy and yam-based products.
Synthetic Hormones are created in a lab and are a close match to bioidentical. These are available by prescription or over-the-counter.
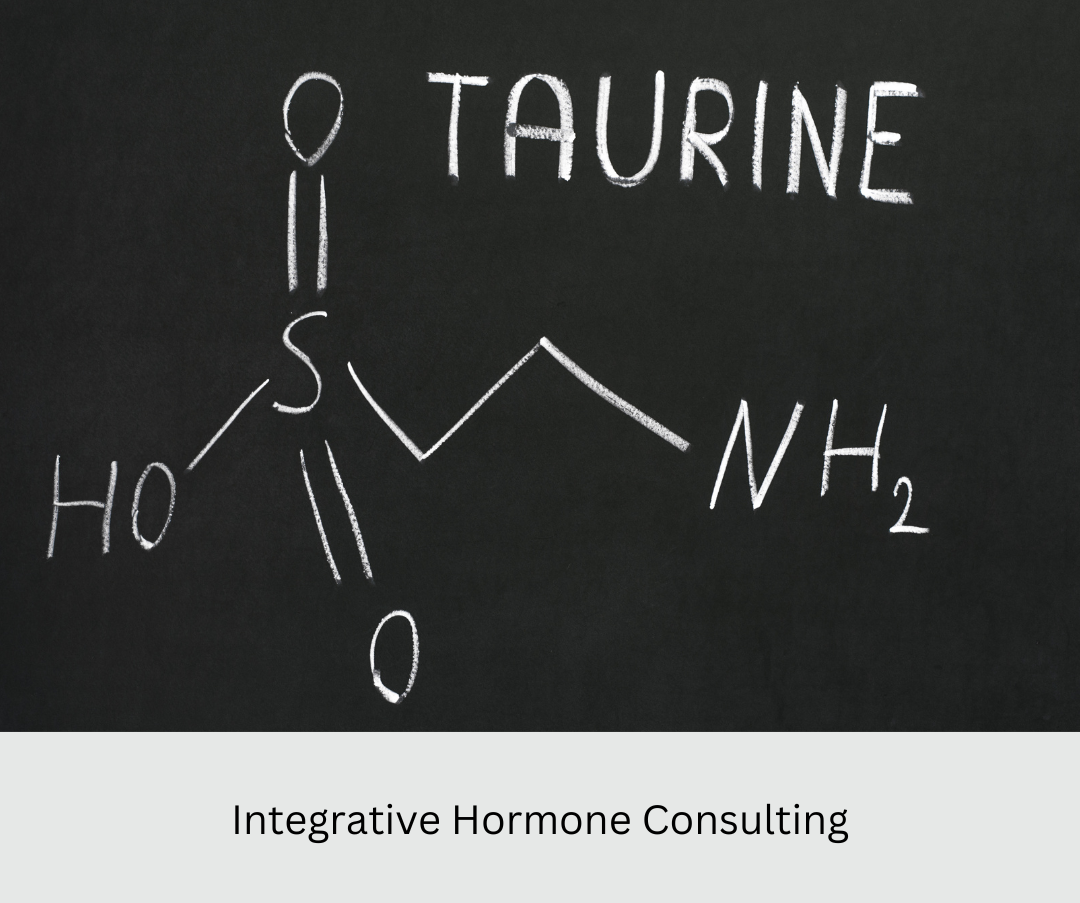
Bioidentical Hormones (Bi-HRT) are identical in chemical and molecular structure to hormones made by a woman’s body. They have been prescribed by doctors for years, are easily adjusted to a woman’s individual needs, and may be based on a panel of hormone tests. Many formulas are available from retail pharmacies and formulary (compounding) pharmacies, which create custom products based on a physician’s order. The molecules for which we generally seek replacement include progesterone, testosterone, DHEA, and three types of estrogen (estrone, estradiol, and estriol).
How do Bioidentical Hormones Work?
The body is swimming in hormones that act like keys in a lock. Basically, hormones are comprised of a solid steroid base decorated with “arms” and “legs.” These attachments turn hormones into specialized molecules (the keys), which plug into receptor molecules (the locks), triggering biochemical reactions in the body. If hormonal replacement therapy doesn’t follow the design our cells have evolved to recognize, women may experience side effects ranging from general discomfort to increased risk for serious illnesses.
How are Custom Bioidentical Hormones Made?
A healthcare practitioner begins with a saliva or blood test to assess hormone levels and ascertain a “recipe” for Bi-HRT unique to the patient. That formula is filled as a prescription by a compounding pharmacy, which is regulated by each state.
Is Bi-HRT a Safer, More Effective Alternative to Conventional HRT?
The long-term study, Women’s Health Initiative (WHI), looked at combined estrogen and progestin for preventing later-life illness. In 2002, the study was stopped because hormone users had a higher risk of breast cancer, heart disease, stroke, and blood clots. Fearful of these results, many women and their doctors concluded they must discontinue hormone therapy. For these women, hot flashes, sleeplessness, and other menopausal symptoms returned with a vengeance. However, it should be noted that conventional HRT is considered an effective approach and studies of Bi-HRT have had promising results; several have gained FDA approval (e.g., Estraderm, Vivelle, Estrogel, Prometrium) and may ease mood, sleep disturbance, anxiety and hot flashes. Bioidentical estrogens are the treatment of choice in Europe and becoming more widely used in the U.S.
Not every woman needs HRT, nor does every doctor recommend it. This is best decided on an individual basis between each woman and her holistic health care doctor.